Introduction
Welcome to Sexsmith Physiotherapy's resource on Calcific Tendonitis of the Shoulder.
Calcific tendonitis of the shoulder happens when calcium deposits form on the tendons of your shoulder. The tissues around the deposit can become inflamed, causing a great deal of shoulder pain. This condition is fairly common. It most often affects people over the age of 40.
This guide will help you understand:
- what happens in the shoulder with calcific tendonitis
- what tests will be run to diagnose this condition
- what you can do to help relieve the pain
- Sexsmith Physiotherapy’s approach to rehabilitation
#testimonialslist|kind:all|display:slider|orderby:type|filter_utags_names:Shoulder Pain|limit:15|heading:Hear from some of our patients who we treated for *Shoulder Pain*#
Anatomy
Which part of the shoulder is affected?
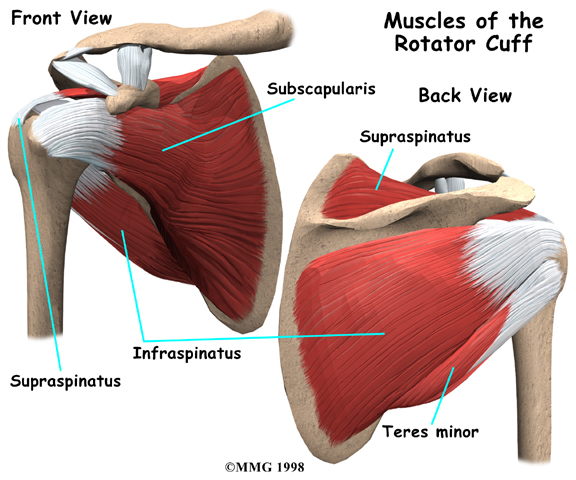
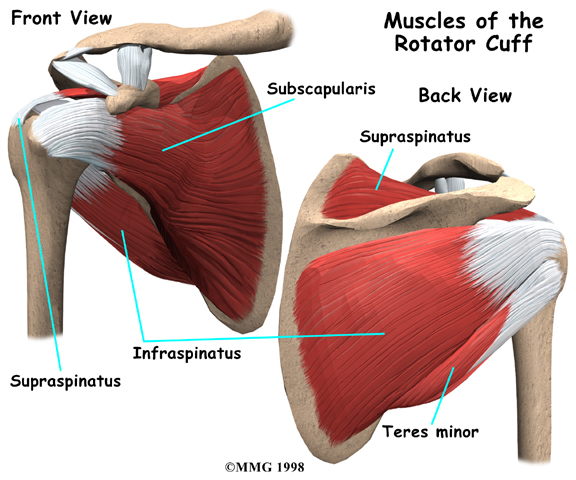
Calcific tendonitis occurs in the tendons (tendons attach muscles to bones) of the rotator cuff. The rotator cuff is actually made up of several tendons that connect the muscles around your shoulder to the humerus (the larger bone of the upper arm).
Calcium deposits usually form on the tendon in the rotator cuff called the supraspinatus tendon.
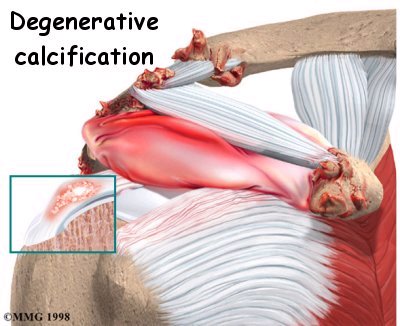
There are two different types of calcific tendonitis of the shoulder: degenerative calcification and reactive calcification. The wear and tear of aging is thought to be the primary cause of degenerative calcification. As we age, blood flow to the tendons of the rotator cuff decreases. This makes the tendon weaker. Due to the wear and tear as we use our shoulder, the fibers of the tendons begin to fray and tear, just like a worn-out rope.
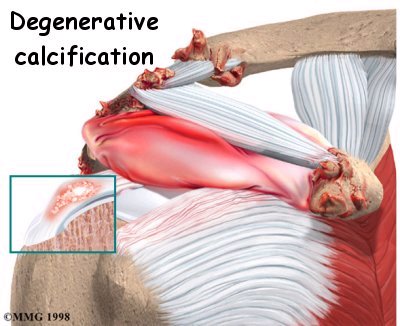
Calcium deposits form in the damaged tendons as a part of the healing process.
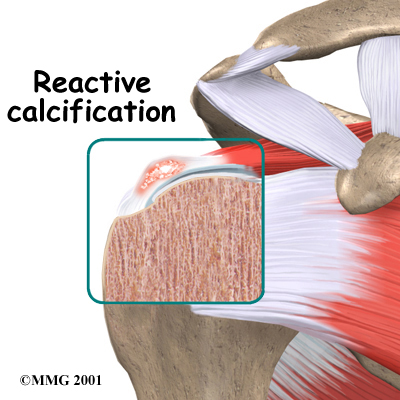
Reactive calcification is different. Why it occurs is not clear. It doesn't seem to be related to degeneration, and is more likely to cause shoulder pain than degenerative calcification. Doctors describe reactive calcification in three stages. In the pre-calcific stage, the tendon changes in ways that make calcium deposits more likely to form. In the calcific stage, calcium crystals are deposited in the tendons then they begin to disappear. The body simply reabsorbs the calcium deposits. Ironically, it is during this stage that pain is most likely to occur. In the post-calcific stage, the body heals the tendon, and the tendon is remodeled with new tissue.
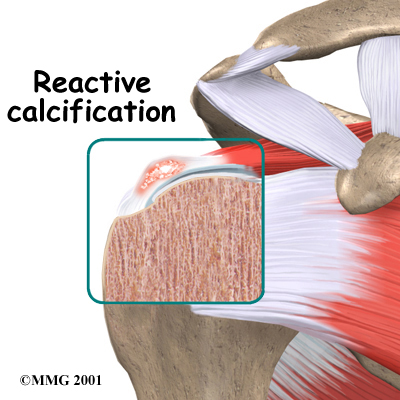
No one knows what triggers the body to reabsorb the deposits, but once this occurs and the tissue begins to be remodeled, the pain usually decreases or goes away altogether.
Related Document: Sexsmith Physiotherapy's Guide to Shoulder Anatomy
Shoulder Anatomy Introduction
Causes
Why did I develop calcific tendonitis?
No one really knows what causes calcific tendonitis. With degenerative calcification severe wear and tear, aging, or a combination of the two are involved. Some researchers think that calcium deposits form because there is not enough oxygen to the tendon tissues. Others feel that pressure on the tendons can damage them, causing the calcium deposits to form.
Reactive calcification is even more of a mystery. This type of problem occurs in younger patients and seems to go away nearly all by itself in many cases, although
Physiotherapy is usually useful to ensure the shoulder pain completely disappears.
Symptoms
What are the symptoms of this condition?
While the calcium is being deposited, you may feel only mild to moderate pain, or even no pain at all. For some unknown reason, calcific tendonitis becomes very painful when the deposits are being reabsorbed. The pain and stiffness of calcific tendonitis can cause you to lose motion in your shoulder. Even lifting your arm may become painful. At its most severe, the pain may interfere with your sleep.
Diagnosis
What tests will my doctor run?
Your doctor will take a detailed medical history and do a thorough physical exam of your shoulder. The pain of calcific tendonitis can be confused with other conditions that cause shoulder pain. An X-ray is usually necessary to confirm the presence of calcium deposits. The X-ray will also help pinpoint the exact location of the deposits.
You will probably need to get several X-rays over time. This will help your doctor keep track of the changes in the amount of calcification. By following the changes in the calcium deposits, your doctor can determine whether the condition will heal with physiotherapy treatment or perhaps require surgery.
Treatment / Rehabilitation
How can I get my pain under control?
Nonsurgical Treatment
Your doctor's first goal will be to help control your pain and inflammation. Initial treatment is likely to be a short amount of rest and also anti-inflammatory medication, such as ibuprofen. The anti-inflammatory medicine is used mainly to control pain. Your doctor may suggest a cortisone injection if your pain remains severe even after trying other nonsurgical treatments. Cortisone is a very powerful steroid. Cortisone can be very effective at temporarily easing inflammation and swelling.
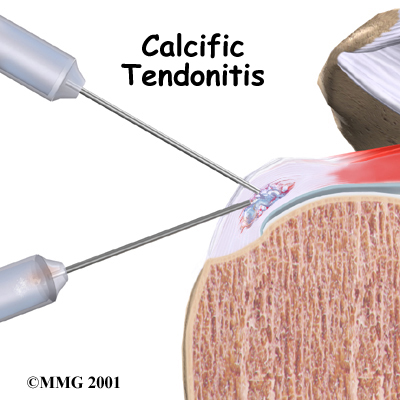
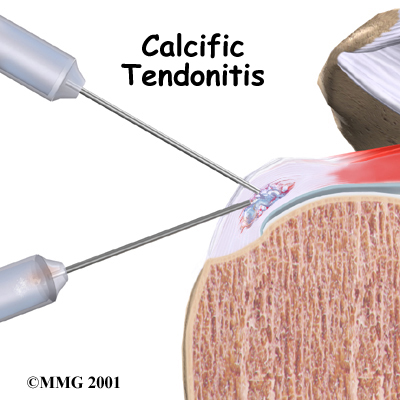
During the time when the calcium deposits are being reabsorbed, the pain can be especially bad. Your doctor may suggest a procedure called lavage in which an attempt is made to try to remove the calcium deposit by inserting two large needles into the area and rinsing with sterile saline (saline is simply a saltwater solution.) Sometimes lavage breaks the calcium particles loose and they can then be removed with the needles. Getting rid of the calcium deposits can help speed up the healing. Even when lavage fails to remove calcium deposits, it may reduce pressure in the tendon, leading to less pain.
Shock wave therapy is another form of nonsurgical treatment. It uses a machine to generate shock wave pulses to the sore area. Patients generally receive the treatment once each week for up to three weeks. The impulses are thought to help break up the deposit so the body can more easily absorb it. Recent studies indicate that this form of treatment does help ease pain and reduce the size of the deposit.
Physiotherapy at Sexsmith Physiotherapy can also greatly assist with controlling your pain and inflammation, and will be crucial to ensuring that you recover the range of motion, strength, and control of your shoulder if you have been diagnosed with calcific tendonitis.
Nonsurgical Rehabilitation
On your first visit to Sexsmith Physiotherapy, your physiotherapist will take a history of your injury and focus on finding out which movements in your everyday life, such as sleeping, reaching overhead or reaching behind your back, cause you discomfort. If you have already seen your doctor and had an x-ray, the diagnosis should be clear. If you have not seen your doctor, then we will further assess your ability to move your shoulder into different ranges of movement, as well as check the strength and stability of your shoulder to help us decide that your pain is indeed caused by calcific tendonitis. Once calcific tendonitis is suspected, we will send you to your doctor to get an x-ray to confirm the problem.
Due to the different types of calcific tendonitis and because of the progressive stages of reactive calcific tendonitis, your pain level may vary. Physiotherapy can be very effective in decreasing the pain as well as the inflammation caused by this injury. Your physiotherapist may use electrical modalities for this purpose. Ultrasound is particularly useful for this and can even decrease the size of the calcium deposit in some cases, although it may require several treatments to do so (4X a week for 6 weeks has been recommended.) Heat and/or ice can also be very useful in decreasing pain and inflammation, as can other modalities such as interferential current. Your physiotherapist may also use massage around the shoulder to ease your discomfort and assist with the associated inflammation.
The next part of our treatment will focus on regaining the range of motion, strength, and coordination in your shoulder. Your physiotherapist at Sexsmith Physiotherapy will prescribe a series of stretching and strengthening exercises that you will practice in the clinic and also learn to do as part of a home exercise program. Due to the initial pain you may feel, the range of motion exercises will first be done passively, which means that you do not use your own muscles of the injured shoulder to lift the joint into its full ranges of motion. Maintaining passive range of motion is particularly important in the early stages of treating calcific tendonitis because the pain associated with this injury often limits you from using the shoulder above shoulder height. If, however, you do not passively maintain the overhead range in your shoulder then your shoulder is at significant risk of becoming stiff and not being able to move into this range even once the acute pain and inflammation caused by the calcific tendonitis has disappeared.
Passive range of motion exercises may include the use of rehabilitation equipment such as pulleys and poles, or your therapist may just ask you to use your non-painful arm to move your painful one. In some cases your physiotherapist themselves may move your shoulder for you; again, this is considered passive motion. An upper body bike may also be useful in the early stages of rehabilitation to improve range of motion and encourage coordinated movement of the entire upper limb, as long as it can be used without causing discomfort.
In order gain strength in your rotator cuff muscles of the shoulder joint, as well as the other supporting muscles of the shoulder, your physiotherapist at Sexsmith Physiotherapy will also prescribe specific strengthening exercises which may, depending on your stage of injury, initially only involve isometric strengthening. Isometric strengthening exercises involve tightening your muscles without actually moving the associated joint. Isometric exercises work the muscles without straining the injured or painful tissues. Your physiotherapist will teach you how to use your other hand or wall for resistance while you flex and tighten your muscles, creating an isometric contraction of the shoulder muscles. Your therapist will then progress your exercises so that you are strengthening the muscles through their available ranges of motion. This may involve using light-weights or Theraband to add resistance for your upper limb. Adequate strength and endurance in the rotator cuff muscles throughout a variety of ranges of motion, including over shoulder height, is needed to ensure full functioning of the shoulder. Adequate strength will also decrease the pressure on the calcium deposits in the shoulder, which may lead to less pain and a quicker recovery.
A crucial component to any shoulder rehabilitation program is the ability for you to regain what is called ‘proprioceptive control’ of your shoulder joint. Proprioception is the ability to know where your body is without looking at it. For example, normally each time you reach overhead with your hand, your mind does not consciously have to think about doing the action, yet all the muscles of the shoulder (and elbow, wrist, and upper back) coordinate the action just right so you can perform the movement without any discomfort or pinching. When you have pain in a joint, or the tissues of the joint have been injured, your proprioception declines. Any period of decreased mobility of the joint will also add to this decline. If the proprioceptive control of your shoulder is poor then the ability to use your shoulder naturally in all ranges of movement without causing any pain or pinching, or unnecessary motion, declines, and your shoulder is at risk of increased wear and tear, and developing another injury. The joint between your shoulder blade and your thoracic spine (called the scapulothoracic joint) is particularly important to the overall proprioceptive control of the shoulder joint. The outer edge of the shoulder blade actually creates the socket of the shoulder joint. Together, the scapulothoracic joint and the shoulder joint itself (including the rotator cuff muscles) create the complete shoulder girdle; the entire shoulder girdle must operate together for normal shoulder motion. Controlled shoulder girdle motion along with adequate rotator cuff strength keeps the ball of the shoulder joint properly centered in the socket of the joint and avoids any pain or undesired motion of the joint. This control and strength is particularly essential when using your limb near or above shoulder height and especially during rapid or repetitive arm movements such as throwing.
For this reason, your physiotherapist will teach you how to properly control your shoulder girdle during your rehabilitation exercises but will also educate you on transferring this control to your everyday activities. Again, this will prevent excessive wear and tear on your shoulder joint even during the repetition of normal everyday tasks.
As you improve in your ability to control the shoulder girdle your physiotherapist will introduce more difficult dynamic exercises for your shoulder including exercises that simulate your daily tasks, or if you are an athlete or simply do recreational sport, those shoulder motions that simulate your sport. Simple proprioceptive exercises might include activities such as rolling a ball on a surface with your hand, holding a weight up overhead while moving your shoulder, or pushups on an unstable surface. Advanced exercises may include activities such as reaching for and lowering a weight, ball throwing, catching overhead, or a simulated swimming stroke or overhead volleyball spike.
Finally, as part of your shoulder rehabilitation, your physiotherapist will also remind you about maintaining good shoulder posture at all times even when just sitting or using your upper limb in activities below shoulder height, such as working on the computer. Rounded shoulders in any position crowds the shoulder joint and can lead to overall shoulder impingement, more pressure on the calcified area of your tendon, and poor recovery from the injury or a new episode of shoulder pain. Simple changes in the way you sit or stand and how you use your shoulder, neck and thoracic spine throughout the day can ease your pain and help you avoid further problems.
In addition to rehabilitating your shoulder joint itself, at Sexsmith Physiotherapy we highly recommend maintaining the rest of your body’s fitness with regular exercise even while you recover from the calcific tendonitis in your shoulder. Cardiovascular fitness can be maintained with lower extremity fitness activities such as walking or using a stationary bike or stepper machine. None of these exercises should cause discomfort to your shoulder; if they do, discuss modifying the activity with your physiotherapist.
You will notice improvements in the functioning of your shoulder even after just a few treatments with your physiotherapist at Sexsmith Physiotherapy. Full recovery, however, will require consistent treatment for approximately 6 weeks. Your home exercise program will likely need to be continued for 3-4 months or longer. If your shoulder joint is not recovering as your % physiotherapist% would expect it should, or if your pain becomes unmanageable, your physiotherapist will suggest that you return to your doctor or see an Orthopaedic Surgeon. More radical treatment measures, such as surgery, may be needed in your case to deal with the calcification.
Sexsmith Physiotherapy provides services for physiotherapy in Sexsmith.
Surgery
If the pain and loss of movement continue to get worse or interfere with your daily life, you may need surgery. Surgery for calcific tendonitis does not usually require patients to stay in the hospital overnight but it does require anesthesia.
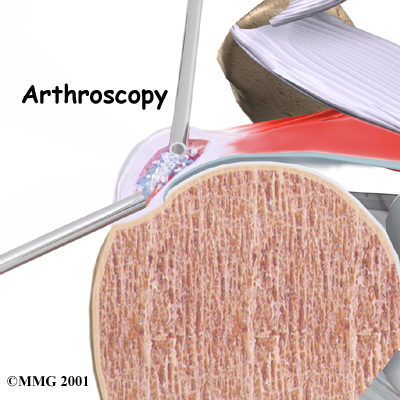
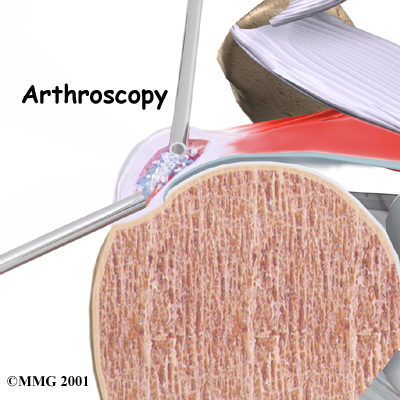
Arthroscopic Resection
Most surgeries to correct calcific tendonitis of the shoulder are arthroscopic surgeries. The arthroscope is a special TV camera that can be inserted into the shoulder joint through a small incision in the skin. Other small incisions allow the surgeon to insert small surgical instruments into the joint as well. The surgeon uses the arthroscope to locate the calcium deposit in the rotator cuff tendon. Once the deposit is found, the surgeon uses the small instruments to resect (remove) the calcium deposits and rinse the area. Loose calcium crystals must be removed. They can be very irritating to the surrounding tissues.
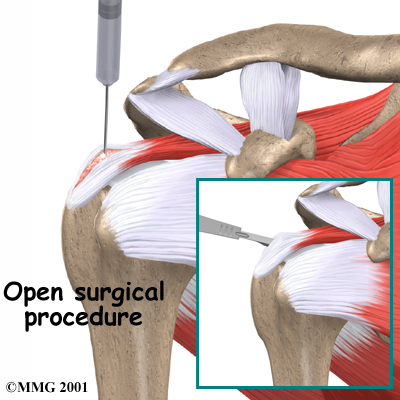
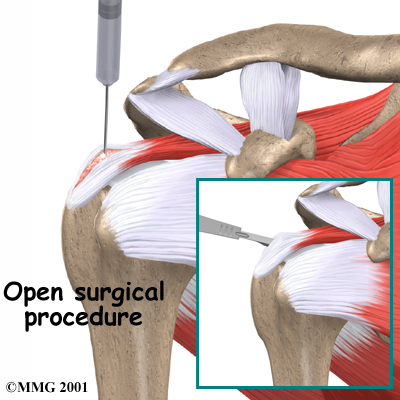
Open Resection
In rare instances, open surgery is necessary. In open surgery, the surgeon gets to the calcium deposit by cutting through muscles and other surrounding tissues. The tendon itself is cut to allow removal of the calcium deposits. The surgeon rinses the area to get rid of calcium crystals and then stitches the muscles and skin together.
Post-surgical Rehabilitation
Rehabilitation after shoulder surgery for calcific tendonitis can be a slow process if you have had an open procedure. You will probably need to attend therapy sessions for six to eight weeks, and you should expect full recovery to take three to four months. Getting the shoulder moving as soon as possible is important, however, this must be balanced with the need to protect the healing tissues. Your physiotherapist will guide you through the appropriate exercises at the appropriate time and ensure that you are advancing your exercises as quickly as you can without compromising the surgical site. Recovery from an arthroscopic surgery for calcific tendonitis will go much quicker and the shoulder should be moving well even within 2-3 weeks.
You may have to wear a sling to support and protect the shoulder for a few days after surgery whether you have had an open or arthroscopic procedure. Your surgeon or physiotherapist will advise you when it is safe to stop using the sling.
Good posturing and adequate shoulder proprioception (also discussed in detail above under non-surgical rehabilitation) is also crucial to post-surgical rehabilitation. Crowding the shoulder joint with slouched posturing or poor shoulder girdle control will add pressure to the tendons that have been cleaned up in the surgery and will lead to ongoing inflammation, pain, and wear and tear in the shoulder joint.
As stated above physiotherapy goes slower after open surgery, where the shoulder muscles have been cut. During the initial few treatments after surgery at Sexsmith Physiotherapy your physiotherapist may use ice and electrical modalities to help control pain and swelling from the surgery. They may also use massage and gentle mobilizations of your joint to ease any muscle spasm and pain.
Your physiotherapist will prescribe early range-of-motion exercises however the range or motion may seem quite limited even for the first couple of weeks, especially in the end ranges of motion such as reaching over-shoulder height or behind your back. Range of motion exercises will first be done passively, which means you will use either your other arm to lift your surgical arm, or a pulley or pole to do the lifting rather than the muscles of your surgical shoulder. Your physiotherapist may also do some passive stretching of your joint even in the early stages of your rehabilitation. Early passive movement of your shoulder joint into the maximum ranges of motions is crucial to full recovery of your shoulder joint after surgery. Proper posture during the passive range of motion exercises will help the shoulder joint move most naturally and avoid any secondary pain and impingement. As you are able, your physiotherapist will advance your exercises so that you actively use your own muscle power to take your shoulder into the different ranges of motion.
Strengthening your shoulder after surgery will begin early on but with only light isometric strengthening exercises similar to those described in non-surgical rehabilitation. Your shoulder joint should not move during isometric exercises, hence why they can be done early on post-surgically and do not harm the healing tissue. Pain should be used as a strict limit during these exercises.
At approximately 3-5 weeks post-surgically you will be able to start doing heavier strengthening as long as your surgeon approves. Light weights or Theraband may be used at this time to increase the resistance for the shoulder, and the exercises will be done throughout the available range of your shoulder joint, including the over-shoulder-height or over-head ranges of motion. Again, as mentioned above, adequate shoulder proprioception is crucial while strengthening the shoulder, so significant time during your rehabilitation sessions at Sexsmith Physiotherapy may be spent perfecting your shoulder girdle control.
As your shoulder strength improves, your physiotherapist will start to introduce exercises that simulate the activities you regularly participate in, whether that be sporting activities, or work-related activities such as lifting or prolonged desk work. As you improve, you will no longer need to regularly attend physiotherapy at Sexsmith Physiotherapy. Your physiotherapist will become more of a resource, while your home exercise program will be your main form of therapy. As usual, your physiotherapist will keep a close watch on your progression of improvement after surgery, and if you are not improving as we would expect, or your pain is not well controlled during your rehabilitation, we will ask you to return to your surgeon for follow-up to ensure there are no complicating factors impeding your recovery.
Physiotherapy can progress quickly after a simple arthroscopic resection. There will be less pain than in an open procedure so an initial focus on modalities and manual therapy for pain will not be as great, however, any pain that is present will be respected and treated.
Treatments can begin very early after the surgery and will start with range-of-motion exercises and gradually work into active stretching and strengthening. Therapy will be similar to the therapy after an open procedure, but progress will be much quicker. Again, your physiotherapist will be crucial in guiding your progress and ensuring that you don’t do too much, too quickly and that shoulder function recovers as it should post-surgically.
Portions of this document copyright MMG, LLC.
Sexsmith Physiotherapy provides services for physiotherapy in Sexsmith.